What is MIS-C, the weird post-COVID inflammatory thing in kids?
Hello! It’s been a little while since I’ve written a COVID-related post, as I have officially graduated with my PhD and am now back in medical school! (And thus am……. rather busy.) I am a third-year medical student now (if that’s confusing to you, check out this post), and I just finished my pediatrics rotation! While on pediatrics, one syndrome kept coming up over and over again: Multisystem Inflammatory Syndrome in Children (MIS-C). By now it’s well established that kids are at much lower risk of severe COVID infections, but you may have heard mention of a weird, sometimes severe inflammatory thing in kids several weeks after they’ve recovered from COVID, perhaps with the word “Kawasaki” thrown in. So, what exactly is this thing?
The very short, simple, and frustrating answer is: we don’t really know yet. Right now we’re still in the stage of describing what we’re seeing, and have very few answers as to why we’re seeing it. Here’s what we know so far, followed by a little speculation of what could be happening.
A Mysterious Kawasaki-like Illness
In April 2020, reports in the UK started coming out of kids with an illness like Kawasaki Disease, but with some differences. Kawasaki Disease is a relatively rare disorder where blood vessels become inflamed, leading to fever, inflammation in the eyes (red eyes), inflammation in the mouth (red tongue and dry/cracked lips), rashes, and swelling in the hands and feet. The disease can make kids quite sick and can progress to cause peeling of the skin as well as involvement of the digestive tract (vomiting, diarrhea). Often the most severe complication is heart damage (due to inflammation of the blood vessels that bring blood to the heart). The cause of Kawaski Disease is still a mystery; there is some data to suggest it’s triggered by an infection or environmental trigger, but we really don’t know.
Again, Kawasaki Disease is rare (and, for unknown reasons, it is more common in children of Asian ancestry.) In England, only about 5 out of every 100,000 kids under age 5 develop Kawaski disease. That’s why at the beginning of the pandemic, doctors in England were very surprised to see 8 cases of a severe Kawaski-like illness over the course of only 10 days, half of whom had reported family exposure to COVID. Something was up.
Since those initial reports, more reports have come in from all over the world of this weird, sometimes severe inflammatory disease in kids that seems to be associated with COVID. In some ways it looks like Kawasaki Disease, but in some ways it’s very different.
Here's what we know so far about MIS-C:
MIS-C seems to be a post-COVID disorder. Data from New York found that the peak of MIS-C cases came about 31 days after the peak in COVID cases, suggesting that MIS-C is a complication that occurs after the infection has resolved, not during the infection. Another analysis found that 60% of kids with MIS-C were negative for the SARS-CoV-2 PCR test (indicating they don’t have an active infection), but had COVID antibodies (meaning they were previously infected). The lag time of 3-4 weeks coincides with the development of antibodies, which has led to the hypothesis that MIS-C is caused by some sort of weird, dysfunctional immune response to a previous COVID infection, not the infection itself.
MIS-C disproportionately impacts Black and Hispanic children, while Kawasaki Disease disproportionately impacts Asian children. Children with MIS-C are also a little older (average age is 8 years old), while Kawasaki Disease usually impacts kids younger than 5.
MIS-C causes a wide variety of symptoms; more common ones are fever, GI symptoms (abdominal pain, vomiting, diarrhea), rash, inflammation of the eyes, neurocognitive symptoms (confusion, tiredness, headache), and rashes on mucosal surfaces (inside the mouth, etc.).
MIS-C can be a very serious disease, leading to heart damage, kidney damage, shock (not enough blood perfusion to the body), respiratory failure, and death. However, we often notice the most severe cases first, so as the months go on, we may find that MIS-C can be mild as we learn to diagnose it better.
One key feature of MIS-C seems to be inflammation. Markers of inflammation in the blood are elevated in MIS-C cases, and a higher level of inflammation seems to be correlated to more severe disease.
Given that MIS-C can cause a laundry list of symptoms, the official diagnosis is also somewhat of a laundry list. To officially diagnose a child with MIS-C, they must have fever, elevated inflammatory markers in the blood, be sick enough to need admission to the hospital, have damage to at least two organ systems (i.e. signs of both kidney and heart damage, for example), have recent COVID exposure/infection, and no other plausible diagnosis (rule out everything else it could be). Hopefully as we learn more about it, we will have a more precise way of diagnosing it.
And lastly, the good news: thankfully, MIS-C seems to be relatively rare. As with most things COVID, we don’t have an exact number, but one report estimated 2 MIS-C cases per 322 COVID infections in people under age 21. However, given that it can cause so many different symptoms, it’s very possible it’s being under-diagnosed.
Molecular Mimicry: Lessons from Little Women
So what is going on? Why are symptoms showing up after the infection? One possibility is that MIS-C is a disease like rheumatic fever. Rheumatic fever is a weird complication that can occur after your run-of-the-mill strep throat infection. Strep throat is caused by the bacteria Streptococcus pyogenes, which causes a fever and killer sore throat, and sometimes a rash as well (Scarlet Fever). These infections are easily treated by antibiotics, and for most people, that is the end of the story. But for some (usually those who weren’t treated or were under-treated), a few weeks after the infection, rheumatic fever can develop. The symptoms of rheumatic fever have nothing to do with the initial infection: they can include arthritis, heart damage, and even neurological disorders, and can lead to long-term health problems and even death.
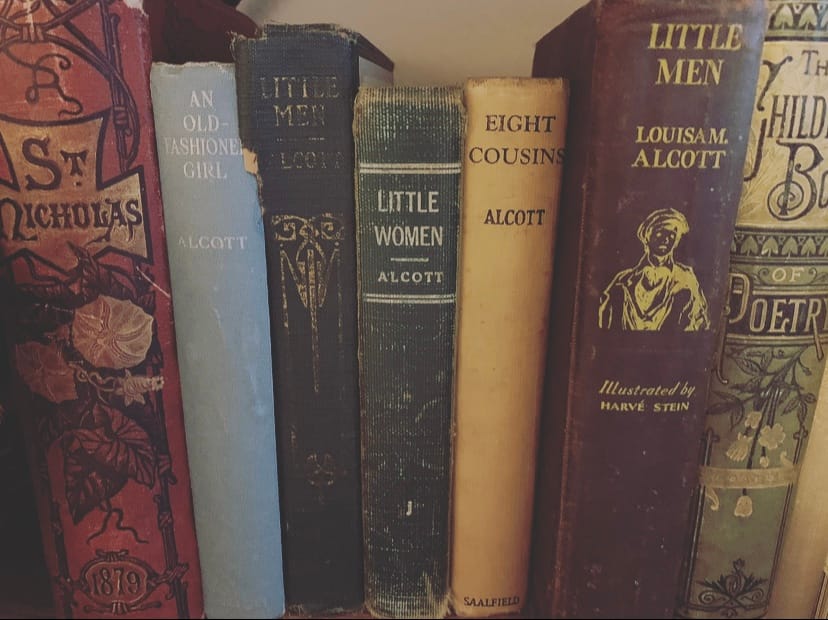
For the Louisa May Alcott fans, this may sound familiar as it is very likely what happened to Beth March in the story Little Women. Beth contracts Scarlet Fever early on in the story (unfortunately she lived in the era before antibiotics were discovered) and seemed to make a full recovery. But then slowly, she gets very, very sick, and ultimately passes away. While it’s not explicitly stated in the book, the course of her illness describes the progression of rheumatic fever (most likely rheumatic heart disease) — ultimately, her heart likely failed. Why did this happen?
Unlike MIS-C, we’ve had centuries to learn about rheumatic fever. It is caused by the immune response to a strep infection, not the infection itself. Our immune systems work by recognizing very specific pieces of bacteria and viruses, then making antibodies and immune cells that recognize those specific pieces and attack them if/when the microbes ever come around again (check out this post for a more detailed description of how this happens). It just so happens that some of the pieces of Streptococcus pyogenes happen to look very similar to pieces of human cells. Poor Beth didn’t have access to antibiotics, so her immune system had to do all the heavy lifting and created a very strong immune response to the Streptococcus pyogenes causing her Scarlet Fever. She beats the infection, but her antibodies are circulating in her body for life, looking for more Streptococcus pyogenes to attack. They come across her heart cells that have molecules that look so, so, so similar, and mistakenly attack them instead. This is called molecular mimicry: two unrelated molecules just happen to be very, very similar in shape, and the immune system can’t tell the difference. Ultimately, this immune response destroys her heart (and our hearts as well 😓).
This may sound alarming — aren’t our immune systems supposed to be super precise? How can they get molecules mixed up? Yes, our immune systems are super precise. It is incredible how good they are at what they do. However, when you consider the millions of different pieces of microbes that our immune systems have to learn to recognize (we are CONSTANTLY exposed to microbes), it’s not so surprising that every now and then, there might be a problem like this. Just like every now and then, two completely unrelated people happen to look nearly identical.
The same thing could be happening in MIS-C: perhaps some molecule on SARS-CoV-2 just so happens to be the EXACT same shape as some other molecule on healthy human blood vessels, causing COVID antibodies to attack healthy human cells after the infection has resolved. But we really don’t know — for now, this is just a guess and one of several possible explanations. It could be molecular mimicry is at play, or it could be something else related to the COVID infection and its impact on the immune system. One case report detected actual virus in the damaged heart cells of a child with MIS-C, suggesting the MIS-C could be a direct effect of the viral infection; however this may simply be due to misdiagnosis of severe COVID infection as MIS-C in that particular patient. COVID is a really, really weird disease. I am studying for my pediatrics exam right now, and it’s striking to me how few infectious diseases affect as many organ systems in the body as COVID does. It will likely be some time before we fully understand this virus and how it impacts the human body.