Misinformation, or miscommunication?
Last week, I wrote about the importance of empathy, listening, and trying to genuinely understand those who distrust public health instead of automatically dismissing or fact-checking them.
To continue in this vein, I am resharing a series I wrote last year (originally published on my Health (Mis)communication column for Your Local Epidemiologist) looking back at the COVID vaccines and dissecting some of the communication problems around them.
The goal of this series is not to lay blame on scientists or the public, but to help the scientific and public health world step outside our bubbles and get a fuller view of why so many distrusted the COVID vaccines. I hope you'll join me for the ride, keep an open mind, and at the end of the day, have a little more empathy for the people who felt betrayed by public health during the pandemic.
The Covid-19 vaccines are undoubtedly among the most impressive medical feats in history. One model estimated that Covid-19 vaccines prevented 20 million deaths worldwide in their first year alone. As a physician-scientist, watching the scientific world come together to produce not one but multiple vaccines in a matter of months in the midst of a global pandemic has been truly awe-inspiring.
But that is not how many people remember them.
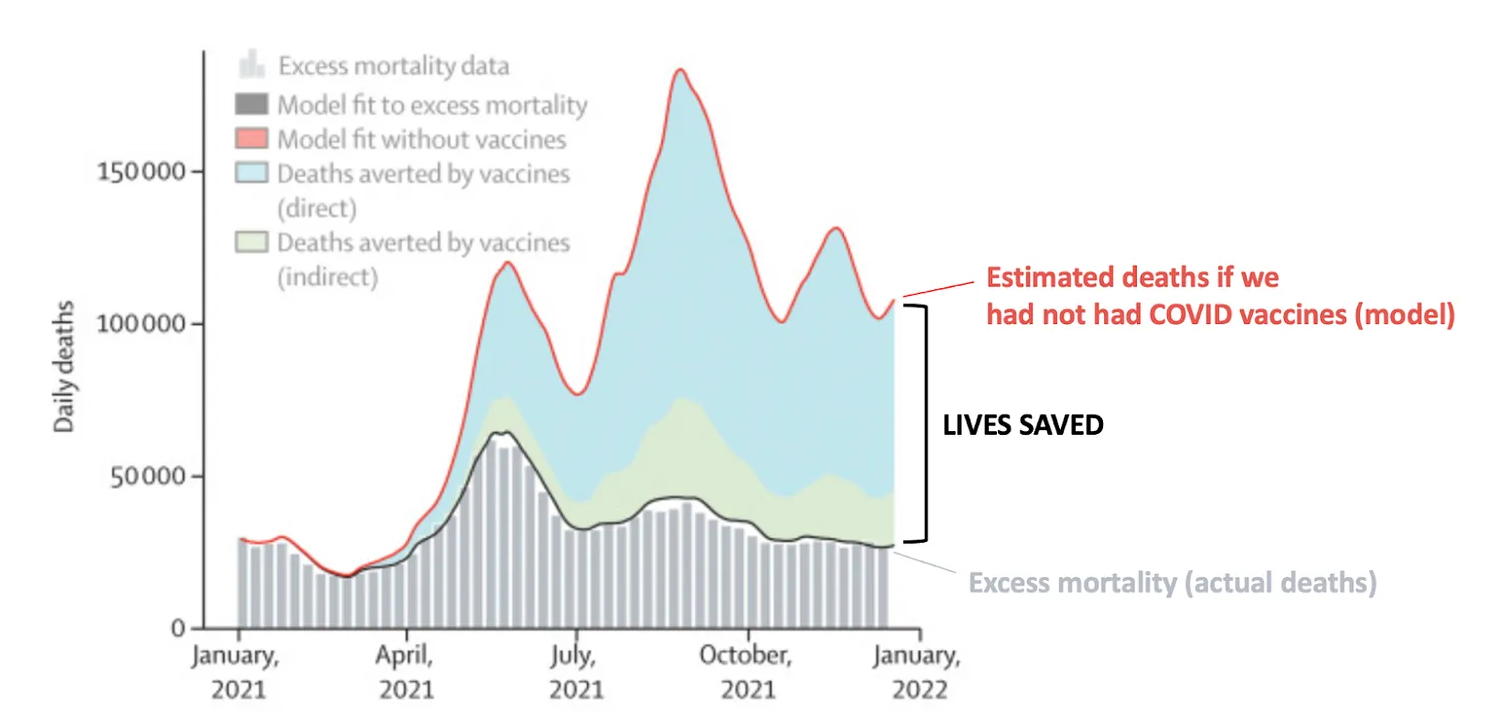
Despite developing multiple effective vaccines that saved millions of lives during a global pandemic, trust in vaccines, even beyond Covid-19 vaccines (like routine childhood vaccinations) got worse, not better.
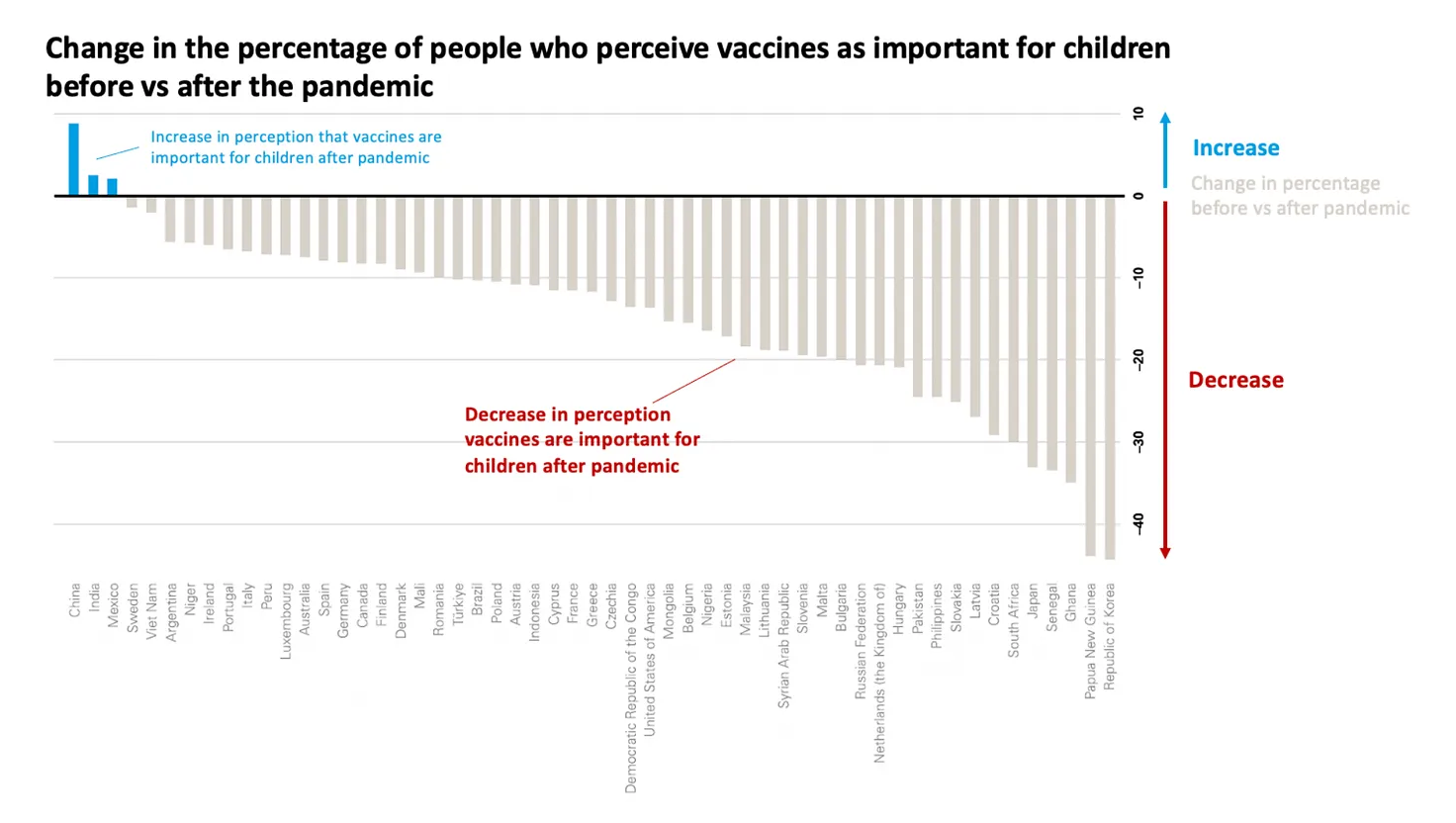
Misinformation played a huge role, but it was not the only problem
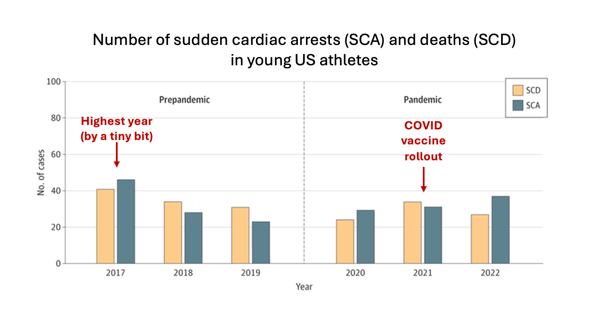
It’s easy to blame it all on misinformation and disinformation, which undoubtedly played a role. The list of rumors about the Covid-19 vaccines is certainly impressive—every week, there was a new alleged “ingredient” that was somehow toxic, and the level of creativity that inspired the various false rumors would be laudable if it weren’t so dangerous.
I’ve spent hundreds of hours debunking various Covid-19 vaccines rumors and don’t want to minimize the impact these rumors had on sowing distrust in vaccines.
But that’s not what this series is about.
Misinformation, or miscommunication?
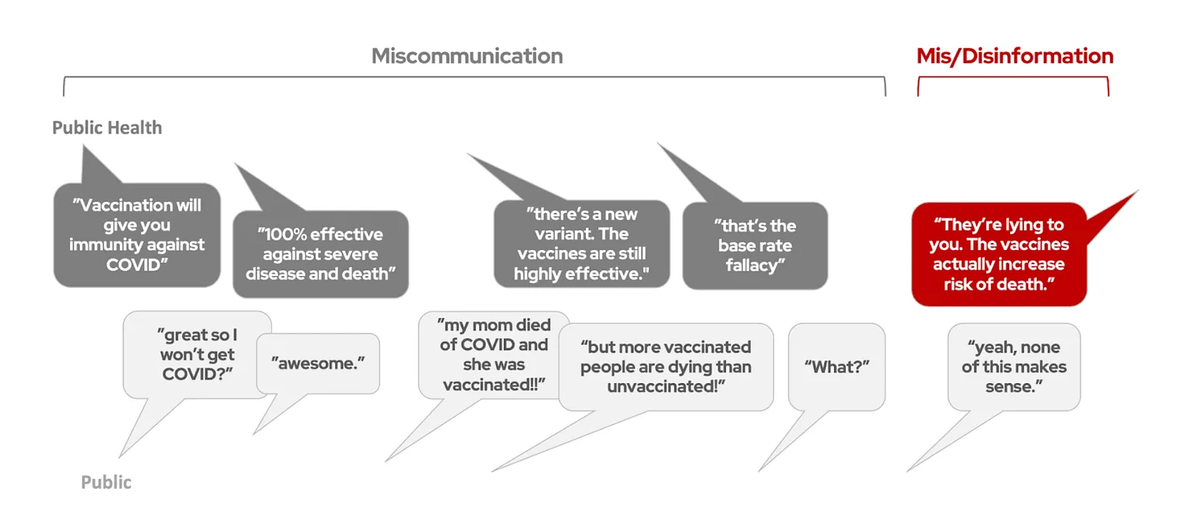
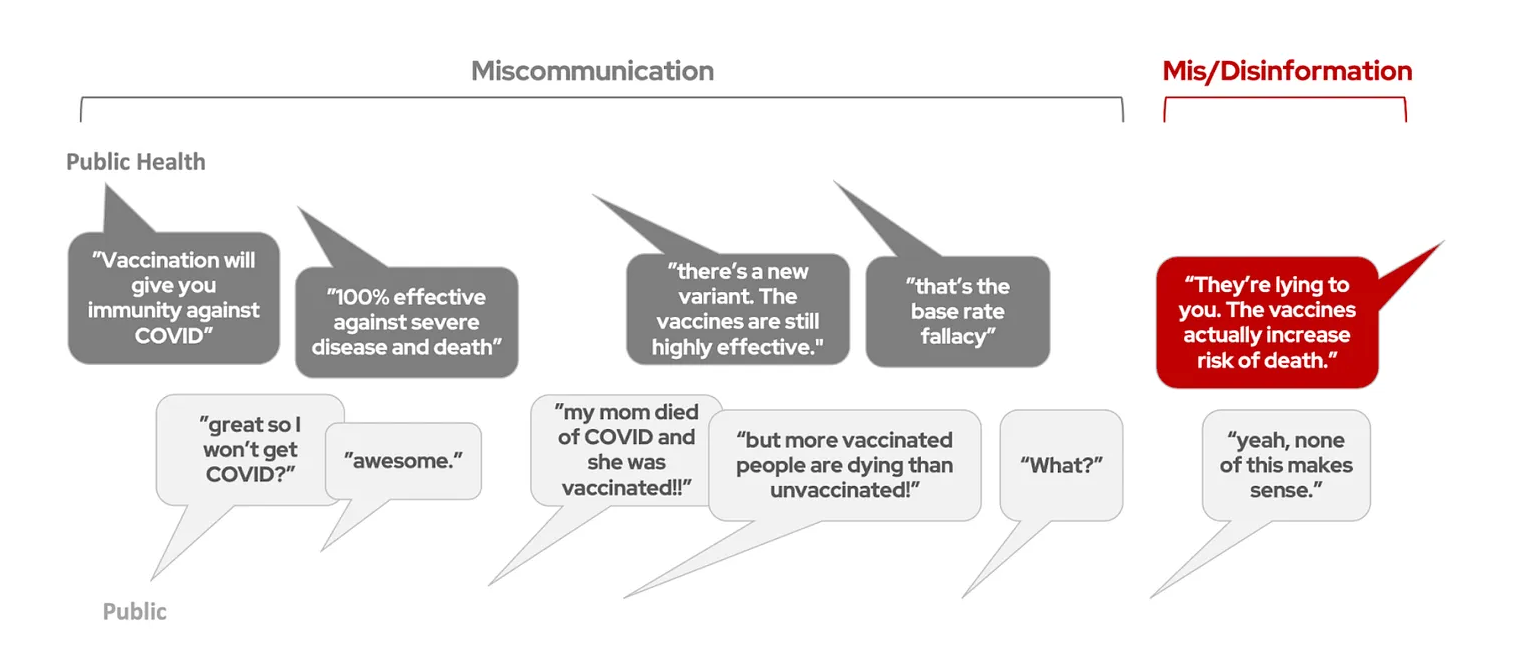
A lot of “misinformation” that was circulating could more aptly be described as “miscommunication”—public health officials saying one thing and the public hearing something entirely different.
- I thought Covid-19 vaccines gave us immunity like our childhood vaccines do—why are vaccinated people getting sick?
- I thought you said all the vaccines give us 100% protection against severe disease and death—why are most Covid-19 deaths now among vaccinated people?
- If the vaccines prevent infection, why do vaccinated people still need to wear masks?
- If I was okay after a Covid-19 infection, am I okay getting measles and other diseases then, too? Are we overreacting?
These are all valid questions that deserve explanations. The answers provided were often confusing, constantly changing, or fell short, leaving the (false) impression in many people’s minds that Covid-19 vaccines don’t actually work, and that the scientific community was pushing a failed vaccine, calling other vaccines into question as well.
Poor communication is a gateway to misinformation
When valid questions aren’t answered adequately or from a place of empathy, it’s not unreasonable that trust declines. And when trust starts declining, people may be more open to believing rumors they hear. Plain old miscommunication can set people on a path to believing misinformation and disinformation.
Misinformation is not going away, and we can (and will) keep addressing rumors as they come. But the generation of these rumors is, for most of us, completely out of our control. In the public health and medicine field, we should be far more interested in looking at what is within our control: our communication, and how we can do better.
The first step is figuring out what went wrong. In this series of posts, we will look back at the story of the Covid-19 vaccines and the communication problems around them. Some pandemic communication blunders were obvious (flip flopping on masks, for example), but others got less attention, and were only obvious to those who were disappointed and confused. The goal is not to point fingers or assign blame—it was h.a.r.d. to communicate to a polarized nation during a deadly pandemic when yesterday’s data was already outdated. But we need to get a view from outside our bubble and understand how messages were perceived, so we don’t miscommunicate next time.
Up next in this mini-series: Expectation management. See you next week.
A version of this article was originally published on Your Local Epidemiologist.
Kristen Panthagani, MD, PhD, is a resident physician and Yale Emergency Scholar, completing a combined Emergency Medicine residency and research fellowship focusing on health literacy and communication. In her free time, she is the creator of the medical blog You Can Know Things and author of Your Local Epidemiologist’s section on Health (Mis)communication. You can subscribe to her website below or find her on Substack, Instagram, or Bluesky. Views expressed belong to KP, not her employer.