COVID vaccination during pregnancy

Guest post by Sana Zekri, MD, a board-certified physician in Family Medicine with Obstetrics.
Rumors about COVID vaccination and alleged impacts on fertility have been circulating since before the vaccines were even available. Because the initial vaccine trials did not study pregnant women specifically, when the vaccines were first authorized, we didn’t have a complete picture about the risks and benefits of COVID vaccination for pregnant women.
Now, over a year later, we do.
In my last post, we discussed the risks and benefits of vaccination for women aren’t yet pregnant, but want to become pregnant in the future. In this post, we’ll tackle the data on COVID vaccination for women who are currently pregnancy or breastfeeding.
Vaccines are a critical tool for achieving healthy pregnancies
Because some viral infections increase the risk of fetal malformations (birth defects) during pregnancy, vaccines are a critical tool for achieving healthy pregnancies. Infections with rubella, zika, toxoplasmosis, human herpesvirus, varicella, syphilis and cytomegalovirus during or near pregnancy can all cause severe malformations. (Thankfully, our data so far suggests that like other coronaviruses, COVID-19 infection does not appear to increase the risk of fetal malformations). Vaccines exist for several of these viruses and are historically known to be protective against disease in pregnancy though most women are vaccinated in childhood and maintain their immunity through child-bearing age. Analysis of vaccination with mRNA vaccines (Pfizer and Moderna) and the adenovirus vector vaccines (Johnson and Johnson) has not been found to increase the risk of fetal malformations. Data suggests no link between COVID vaccination and other problems that can occur in pregnancy including preterm birth, small for gestational age babies, high blood pressure, and gestational diabetes.
Is there any connection between COVID vaccines and miscarriage?
Before we discuss vaccines, it’s important to mention that miscarriage (loss of pregnancy at less than 20 weeks) is unfortunately very common. About 1 in 3 pregnancies end in miscarriage, usually because of abnormalities of the genetic material that came together to make the baby (which is a function of the ‘quality’ of the sperm and egg as well as an element of chance). There are also a few viruses that increase the risk of miscarriage – one of the most widely known is parvovirus B-19.
Thankfully, we have not seen an increase rate of miscarriage with COVID vaccination. V-safe is a specific database established by the CDC that was set up to monitor for any vaccines side effects in pregnancy. Analysis of the data from V-safe has shown similar rates of miscarriage in vaccinated women vs. historical rates, providing reassuring evidence that the vaccines are not increasing the rates of miscarriage. Another study that looked at the rates of miscarriage for women who got the COVID vaccine in the month before pregnancy also did not find any differences between vaccinated and unvaccinated women. Miscarriage rates in women who have gotten COVID-19 virus or the vaccines appear to be the same as the general population. I personally have not seen a change in the expected rates of miscarriage in my own practice, an anecdotal report that supports these robustly collected data.
How does COVID infection impact pregnant women?
Whenever making a decision about vaccination, it’s always important to weigh the risks against the benefits. If we only think about possible risks from vaccination (or any drug), yet ignore the benefits (protection from disease), then we have an incomplete view. When making a decision about getting vaccinated during pregnancy, the same is true: we weigh the risk of side effects from the vaccine (which are very low) against the risks of complications from COVID infection (which are elevated in pregnancy.)
Women who get COVID-19 during pregnancy, especially in the second and third trimester, are more likely to have severe COVID illness and require hospitalization and ICU care than women who are not pregnant. The INTERCOVID trial looked at women all over the world who contracted COVID during pregnancy and compared them against women who did not contract COVID during pregnancy. The results were very concerning. The risk of having symptomatic COVID was higher in pregnant women compared to non-pregnant women. The risks of developing high blood pressure in pregnancy, needing to go to the ICU, maternal death, problems with the mother or baby that would require early delivery, and stillbirth/newborn death were all increased in women with symptomatic COVID. Women who were asymptomatic but tested positive for COVID still had an increased risk of developing high blood pressure in pregnancy than women who never tested positive for COVID. The risks of blood clots were also found to be higher in pregnant women infected with COVID compared to women who were not infected. Women who recover from COVID-19 illness still have a higher risk of developing high blood pressure of pregnancy and diabetes of pregnancy. These risks may be linked to changes in the blood vessel structure in the placenta that occur as a result of COVID infection. Placental abnormalities also increase the risk of small for gestational age babies, who have higher risks of going to the NICU and death.
Another concern during pregnancy is fever in the first trimester (weeks 1-12), which can increase the risk of fetal malformations. COVID-19 illness, vaccination, or any illness may cause fever, and this increases the risk of fetal malformations. COVID-19 illness typically causes higher fever, for longer, and is associated with more hospitalization and severe illness than vaccination against COVID-19, as pregnant women who got the COVID vaccine typically reported only mild fever.
What about variants and breakthrough infections during pregnancy?
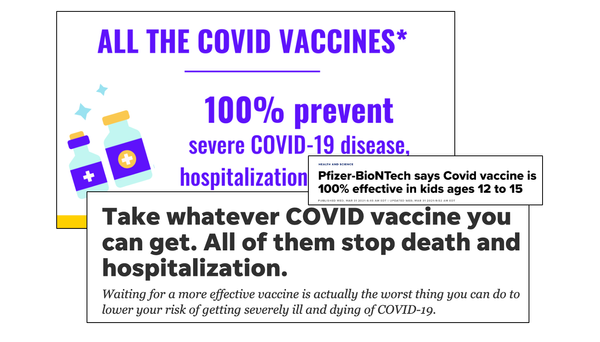
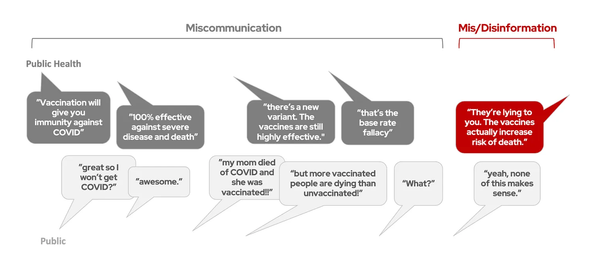
Before we discuss pregnancy specifically, let’s do a quick recap of the efficacy of the COVID vaccines generally. The COVID vaccines were developed against the spike protein of the original SARS-CoV-2 virus. These vaccines showed strong signs of being able to prevent disease with the original virus (informally called the ‘OG’) and the alpha variant. Unfortunately, soon after the COVID vaccine had high enough production to allow for larger scale vaccination in the United States, a more contagious variant became prevalent (delta). The vaccines in our arsenal appeared to be somewhat less effective against the delta variant compared to the OG and alpha variant, but even for the delta variant, people who were unvaccinated still were about 5x as likely to get COVID-19 compared to vaccinated people, and were about 16x more likely to die. Vaccination (especially with a booster) also significantly reduces the likelihood of hospitalization and death from omicron (which is not a ‘mild’ virus) — for the details on vaccine efficacy against omicron, check out this post. So, in short, vaccination provides significant protection against bad outcomes from COVID, even for the variants.
A logical question, especially in the era of the Delta and Omicron variants, would be the impact of breakthrough infections for pregnant women. If you are vaccinated against COVID and still get infected anyway, does the vaccine provide any benefit? A recent study found that pregnant women who were vaccinated and got COVID anyway were much less likely to end up in the ICU or have severe illness. The study wasn’t large enough to detect differences between risks of stillbirth and maternal death, but importantly, all of the 6 stillbirths happened in the infected, non-vaccinated group and the only maternal death was in the non-vaccinated group. This early data strongly suggests that vaccination against COVID reduces the likelihood of adverse outcomes even for breakthrough infections.
Is vaccination safe during breastfeeding?
The vaccine appears to be safe if administered during breastfeeding. A small study showed relatively mild side-effects in mothers who were vaccinated while breastfeeding, though there were a few reports of decreased milk production. Both COVID-19 illness and vaccination create antibodies that are passed on to the baby in the breastmilk. COVID-19 illness appears to produce more variable levels of antibodies, while vaccination produces consistent levels of antibodies. Infection may produce higher initial levels of antibodies compared to people who are getting the first of a two-dose series.
Thankfully, while protective antibodies are passed through breast milk, the virus itself does not appear to pass through the breast milk. Viral particles have not been isolated from breastmilk. A mother infected with COVID does risk passing on the infection to the baby by breathing on the baby, though. Current recommendations about breastfeeding while infected with COVID can be found here.
The benefits of COVVID vaccination far outweigh the risks
Data on the vaccines in pre-pregnancy, pregnancy and breastfeeding show a very good safety profile. Many studies have been performed assessing the safety of COVID vaccines in pregnancy and have discovered that antibodies from vaccination do not attack the placenta and that there is no increased risk of miscarriage, stillbirth, fetal malformations, or preterm birth after COVID vaccination. In contrast, COVID infection does increase the risk of pregnancy complications like need for ICU-level care, stillbirth/newborn death, and other complicating factors. Pregnancy is a risk factor for severe outcomes from COVID, and vaccination helps protect pregnant women from these bad outcomes. The data are clear: vaccination in any of these periods is much, much safer than getting COVID during these periods, for both the mother and the baby.
Dr. Sana Zekri, MD is a Family Medicine with Obstetrics Physician. His particular interests are in public health, global health, women’s health and working towards justice in medicine. He is currently an Assistant Clinical Professor at SUNY Upstate, in Syracuse, New York.
The views expressed on this website do not necessarily reflect the official views of the author’s employers or affiliated institutions. This post is for informational purposes only and is not meant to substitute medical advice from a qualified health professional.