COVID
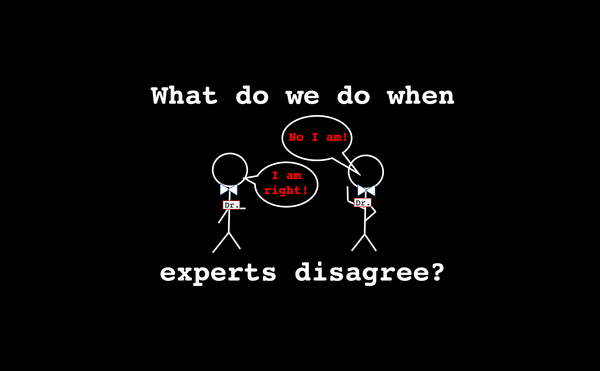
What do we do when experts disagree?
A friend of mine recently asked me how I respond to people who have opposing views about scientific issues like vaccines, and as evidence they cite people with credentials (i.e. PhDs, MDs) who agree with their position. This is a great question, and something I encounter all the time.