If you’re vaccinated, why does it matter if I am not?
With the introduction of the COVID vaccine mandates, one common question has arisen: if vaccination works, then why should the vaccinated care if others don’t get the vaccine? If I’m vaccinated, then aren’t I protected? Why do I need my neighbor to be vaccinated, too? This line of thinking has led some to believe that the vaccines don’t actually work — if they truly worked, they argue, then those who are vaccinated shouldn’t worry about those around them choosing not to get vaccinated. If they are truly protected, then it shouldn’t matter if other people expose them to COVID, so the argument goes.
But, this line of reasoning falls into a type of ‘all or nothing’ thinking that doesn’t capture the reality of what is going on. It is simultaneously true that getting vaccinated helps protect me against COVID, and that it benefits me if my neighbor is vaccinated. These are not mutually exclusive.
There are three major reasons why your decision to get vaccinated impacts the people around you:
- Vaccinated people are less likely to transmit the virus to others.
- Vaccination helps reduce the risk of new variants developing.
- Vaccination reduces the burden on hospitals.
The COVID vaccines work, but aren't 100% perfect
“The COVID vaccines work.” This phrase has been stated over and over, but before we go any further, it’s important to clarify exactly what we mean by “work,” as the communication around this topic has been confusing. Does “the vaccines work” mean that if you get vaccinated, you’re guaranteed never to get COVID?
No.
By saying that the vaccines “work,” we mean that the vaccines significantly reduce the risk of getting infected, hospitalized, or dying. We do not mean that they totally eliminate that risk. Vaccines, like all other medical interventions (and for that matter, most things in life) are not all or nothing. When we say seat belts “work,” we don’t mean that a seat belt is a guarantee that nobody will ever die in a car crash. We mean that compared to not wearing a seat belt, seat belts significantly reduce the risk of severe injury or death in a car crash. If someone was wearing a seat belt and still died in a car crash, we don’t instantly conclude that seat belts are worthless. We conclude that they help in many cases, but aren’t perfect, and this was one of the tragic exceptions.
So yes, the vaccines work, but they are not perfect. A vaccinated person is still at risk of being impacted by COVID, but that risk is much lower than if they were not vaccinated. For a more in depth discussion of breakthrough infections, check out this post.
Reason #1: Vaccination reduces transmission.
Because vaccines are not a 100% guarantee of protection against COVID, my risk of getting COVID is not only impacted by my own vaccination status, but is also influenced by how many people around me are vaccinated. This can be a confusing concept, so here’s an example.
Let’s say there are two friends, Lincoln and Charlie (named after my adorable pets, pictured below.) Let’s say that Lincoln is vaccinated, and Charlie is not. Charlie and Lincoln walk into a room where, unfortunately, someone else with the delta variant had been coughing away moments earlier. There is lots of delta variant in the room, and they are both equally exposed to the virus.


All else being equal, who is more likely to develop symptoms? (To clarify, both are humans in this example.) Definitely Charlie, as he is not vaccinated. Assuming Lincoln got one of the mRNA vaccines, his risk of developing symptoms is ~60% lower than Charlie’s (range in studies is 39-84%), and his risk of ending up in the hospital is 75-95% lower than Charlie’s. Because Lincoln was vaccinated, his immune system had a head start fighting off the virus, so his risk of bad outcomes is much lower. It’s not zero, but it’s much lower. (Due to the range of estimates in the studies evaluating vaccine effectiveness against delta, as well as the strengths and weaknesses of each individual study, it is hard to put an exact number on vaccine effectiveness, which is why ranges are reported. In these types of studies, it’s normal to get some level of variation among the results from different studies. For a detailed discussion on the studies, I recommend reading through this.)
In this situation, does the fact that Charlie is unvaccinated impact Lincoln’s chance of getting sick? No. I think this is where people are getting confused about how other people’s vaccination status impacts them. If I’m standing next to my unvaccinated friend breathing in SARS-CoV-2 particles from a different source, my friend’s vaccination status, in that moment, does not impact my risk of getting COVID from that exposure. That’s not how it works.
My neighbor's vaccination status impacts me
You may be confused, because aren’t people saying that the vaccination status of those around us impacts our risk of getting COVID? Yes it does. To see why, let’s follow Charlie and Lincoln’s story a little further. Charlie (unvaccinated) ends up getting COVID, and Lincoln (vaccinated) doesn’t. But Charlie doesn’t feel sick right away, and keeps going about his day. Pepsi, their friend, meets up with them for coffee. (Pepsi was one of my childhood cats. We had so many animals that we started running out of names, and began naming them after food products. She had an entire litter of kittens with soda-themed names.) While Pepsi, Charlie, and Lincoln are hanging out, Charlie is contagious, but isn’t showing symptoms yet. Lincoln is not contagious, because the vaccine gave him a head start beating the virus, and he killed it off very quickly. Charlie exposes Pepsi to the virus; Lincoln doesn’t.
Vaccination reduces transmission (even for delta)
While multiple factors impact the likelihood that each person becomes infected and transmits the virus after an exposure, vaccination status plays a big role. It is true that vaccine effectiveness against infection and transmission is lower for delta than it was for previous variants. But even for delta, the vaccines reduce the risk of transmission relative to those who are unvaccinated. There has been debate about whether a vaccinated person with a breakthrough infection is just as likely as an infected unvaccinated person to transmit the virus. New data suggests that is not the case. Regardless, even if this were the case, vaccinated people are less likely to be infected in the first place, so they are overall less likely to transmit the virus.
So in large part because Lincoln was vaccinated, he doesn’t expose Pepsi to the delta variant. And in large part because Charlie was unvaccinated, he does expose Pepsi to the delta variant. This is how Lincoln and Charlie’s vaccination status impacts the people around them. Those who are vaccinated are less likely to expose others. Those who are unvaccinated are more likely to expose others.
(You may be thinking, “but what about those who have already been infected with COVID and now have some level of natural immunity? How does that impact the risk of transmission?” It is certainly a fair question, but it’s a whole other complex topic of discussion, and one I hope to tackle in a future post.)
Having more COVID around is worse for everyone
But what if Pepsi is vaccinated? Isn’t she protected? Why should she care if Charlie exposes her, if the vaccine works? Again, because “works” doesn’t mean perfect. Her risk of a bad outcome from COVID is reduced because she’s vaccinated (just like Lincoln’s was), but it’s not eliminated. While her risk of getting COVID is lower because she is vaccinated, her risk would have been even lower if Charlie had not exposed her in the first place. Now that she is exposed, she may not get COVID at all, like Lincoln. Or she may only have a mild infection, but have to miss work. She may pass it on to her unvaccinated child or her immunocompromised sister. Or she may be one of those rare cases who does end up in the hospital. So even if a person is vaccinated, their likelihood of being negatively impacted by COVID is still influenced by the decisions of people around them.
To summarize this simply, there are multiple variables that impact a person’s risk of having a bad outcome from COVID, including 1. whether or not they are vaccinated and 2. how likely they are to be exposed to the virus. The first is entirely dependent on their own actions. The second is in part dependent on their own actions (choosing to social distance, wear a mask, etc.) but is also dependent on the actions of those around them.
We can see this clearly play out on a national level: where there are more unvaccinated people, there is more COVID. The graphs below show the number of COVID cases (left) and deaths (right) per 100,000 in each US county during the summer delta surge on the y-axis, and the percent of each county who was vaccinated at the beginning of the summer delta surge on the x-axis. Counties with lower vaccination rates had higher numbers of cases and deaths. I just spent a month in New England (which has a higher vaccination rate overall), and my risk of getting COVID there was much lower than my risk of getting COVID back home in Texas (which has a lower vaccination rate). My vaccination status did not change; the amount of COVID around me did.
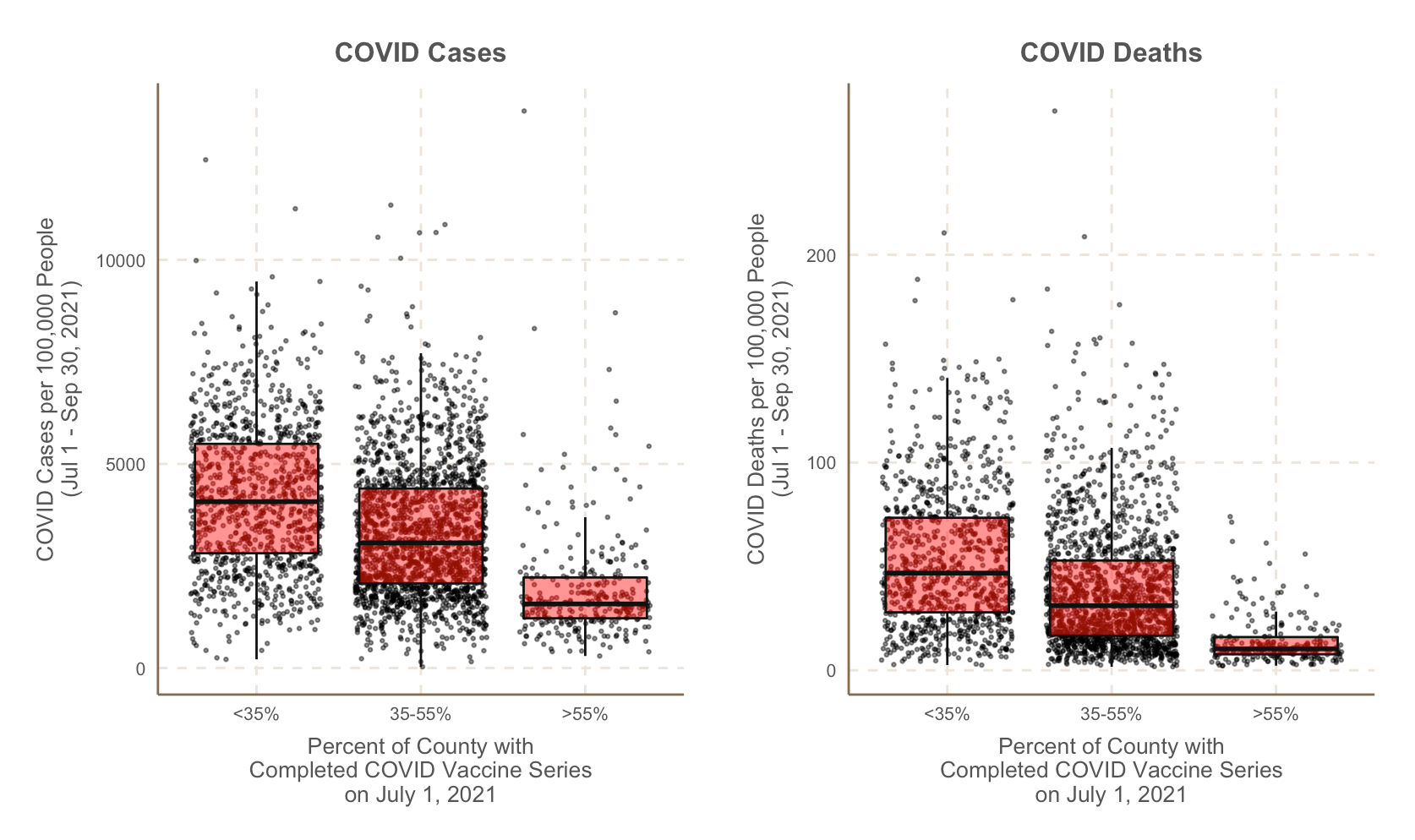
COVID cases and deaths data is from Johns Hopkins, vaccination data is from the CDC.
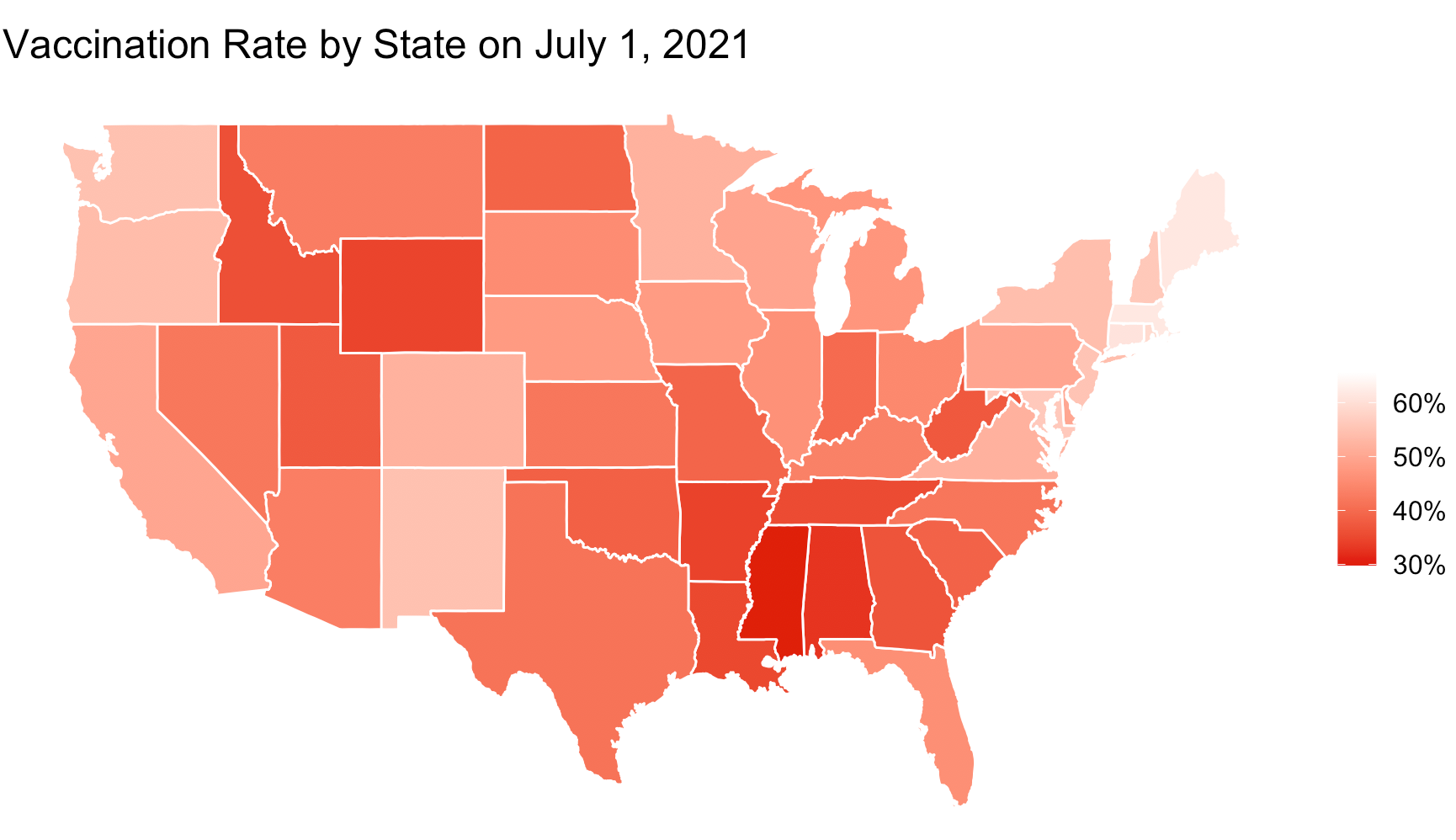
Vaccination data by state from Our World in Data.
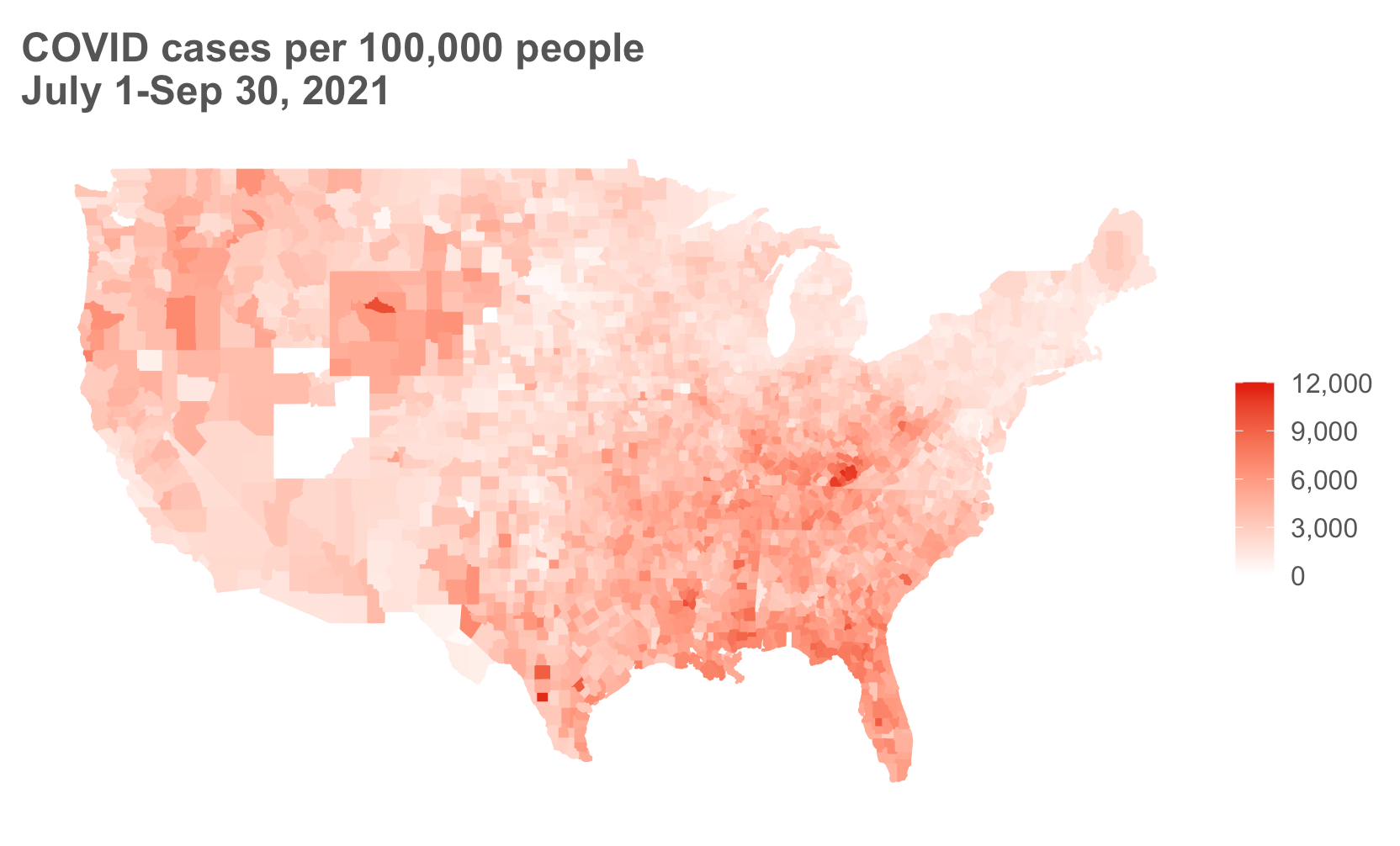
Data from Johns Hopkins.
Reason #2: Vaccination helps decrease the risk of new variants
Increasing transmission is not the only way that the unvaccinated impact the vaccinated; getting vaccinated also helps reduce the risk of new variants developing. There has been a lot of confusion on this one, so let’s clear a few things up.
First, where do variants come from? Variants arise from random mutations in the virus’ genetic code during replication. This is a normal process that occurs in every living organism. The molecular machines that copy the genetic code during replication are not perfect (and RNA viruses like SARS-CoV-2 are even more sloppy at copying), so every time a new copy of the virus is made, there is a new chance for mutations to arise. Not all mutations are bad. Some do nothing, some make the virus worse at being a virus, but a few rare ones will make the virus better at infecting people. The virus cannot “tell” which mutations are going to help it, and then mutate its genome accordingly. It’s just random chance. And the more times the viral genome is copied, the more mutations are produced, and the higher the chance a bad variant will arise.
Where does viral replication happen? Inside human bodies, when someone is infected. So where do new variants come from? Infections. More infected people = more viral replication = more random mutations = more chances for new variants.
Therefore vaccination reduces the risk of new variants arising because, if there are more vaccinated people, there will be fewer infections, which means there are fewer mutations happening. That means that the best way to reduce the risk of new variants arising is by reducing the number of infections. And vaccinations do that.
You may be thinking ‘but what about selective pressure? Don’t vaccines select for vaccine-resistant variants?’ Yes, but that’s not the whole story. Vaccines do not produce vaccine-resistant variants. Vaccine-resistant variants arise by chance and are more likely to arise in a world with fewer vaccinations, because there are overall more infected people (and thus more viral replication and mutations) in that world. But, if a vaccine-resistant variant were to arise because of the high number of infections happening due in large part to lack of vaccination, then yes, selective pressure may favor that variant to spread. But it’s essential to note that vaccination itself does not cause this variant to emerge.
Vaccines are not antibiotics
Some have argued that because vaccine-induced immunity doesn’t always completely destroy every last viral particle, the vaccines are prone to increasing the risk of developing variants that are vaccine-resistant. Some have likened it to antibiotic resistance — if someone has a bacterial infection and they take antibiotics but don’t fully kill off the infection, they are at risk of breeding bacteria that are resistant to that antibiotic. Is this true of the vaccine?
Thankfully, no. This comparison is not accurate because vaccines aren’t drugs like antibiotics, they’re tools that train an entire army of immune fighters. An antibiotic is like a single weapon that attacks the bacteria. The bacteria only need to figure out how to evade that single weapon to develop resistance. Vaccine-induced immunity is like an entire army with a diverse arsenal of weapons — we have a diverse set of antibodies as well as T cell-mediated immunity that attack the virus in different ways. Vaccine-induced immunity creates immune fighters that target different parts of the SARS-CoV-2 spike protein, so even if the spike protein mutates in one place to evade one set of immune fighters, there are other immune fighters that will still be effective. Said another way, vaccine-induced immunity is like taking many different antibiotics simultaneously, not just one. In order to develop resistance during infection, the virus would have to evade all of these at once. This is highly unlikely. So do not worry that getting vaccinated is going to speed up the development of vaccine-resistant variants. It will do just the opposite. Check out these explanations by Edward Nirenberg and Dr. Angela Rasmussen for more details.
Reason #3: With fewer COVID hospitalizations, there are more hospital beds for everyone else
And finally, one of the most critical reasons why my neighbor’s vaccinations status impacts me: hospital capacity. As delta has swept through the country, hospitals have been filling up with predominately unvaccinated patients. This has pushed some hospitals over capacity, requiring them to triage care, cancel surgeries and procedures for other patients, and be unable to provide the full quality of care to other patients needing it. In some cases, the issue isn’t physical space, it’s lack of qualified staff to care of patients. This summer, one in four ICUs in the United States were over 95% capacity. Hospitals have had to send patients hundreds of miles away to find an open ICU bed. And it’s not only COVID patients who are impacted; when the hospitals are full, it impacts everybody’s care. A man in Texas died from gallstone pancreatitis (a treatable condition) due to a delay in care, as they searched across multiple states to find an open ICU bed. A man in Alabama with a cardiac emergency was turned away from 43 ICUs before being transferred out of state. He finally found an ICU that would accept him, but died shortly later. Stories of overwhelmed ICUs across the country have been commonplace this summer. Some ICUs became so full that they allowed “crisis standards of care”, meaning that instead of treating everybody as they normally would, when resources are scarce, they have to choose which patients they are going to treat based on who is most likely to survive. This is not normal. Hospital resources, including beds, equipment, and trained staff, are not infinite, and they can be (and have been) overwhelmed. By choosing to not get vaccinated, the unvaccinated are greatly impacting their community with their choices.
The decision not to get vaccinated impacts both the individual making that decision as well as those around them. If someone chooses not to get vaccinated, they are more likely to transmit the virus to other people, they are more likely to use healthcare resources, and they are more likely to have the virus replicate inside them, which collectively increases the probability of a new variant arising. So even though I am vaccinated, my life is still impacted by the decisions of people in my community.




